Combining PRP and Stem Cells: What Role Does the ECM Play?
Learn about the effects of combining PRP and stem cells and the role of ECM. Learn the benefits of the extracellular matrix (ECM).
The Foundation of Regeneration
PRP and stem cells could be the most popular combinations in regenerative medicine. The combination of them is a biological union that can create new life, revive, and heal. However, in the background of this dynamic duo is a silent partner, the extracellular matrix (ECM), that enables both PRP and stem cells to perform their regenerative magic.
To truly understand how PRP and stem cells work, we need to explore the environment in which they operate.. The ECM is not merely the background structure but the network of communication of healing or transmitting chemical, mechanical, and biological messages that instruct the cells on how to act. ECM + PRP + stem cells combined can create a regenerative triad that is similar to the way the human body heals.
Recent discoveries by Frontiers in Bioengineering and Biotechnology (2025) show that ECM-based scaffolds enriched with PRP and stem cells accelerate bone and cartilage repair more effectively than traditional grafts. The takeaway? The ECM is not merely servicing the process; it is coordinating it.
Understanding the ECM
Consider the extracellular matrix (ECM) as the invisible scaffold that supports each of the tissues. It is made of collagen, elastin, and glycoproteins, and it gives the instructions and structure of the cellular behavior.
The ECM is the first responder when an injury takes place, and it forms a temporary scaffold that attracts the stem cells to the wound site. It also releases biochemical signals, growth factors, cytokines, and enzymes, which direct those cells to differentiate, either into cartilage, bone, or connective tissue.
But as a person gets old or has suffered severe damage, this natural structure becomes weak. Regenerative medicine comes in to re-establish the guiding environment of the ECM through the application of biomaterials and technology.
A decellularized tissue combined with biopolymers has been used to manufacture ECM-mimicking scaffolds. These scaffolds react with PRP and stem cells, enhancing their regenerative property (MDPI Bioengineering, 2024).
Essentially, the ECM performs a translator role in between biology and technology, and makes sure that stem cells get the correct instructions and that the biochemical messages of PRP get to their destination effectively.
Stem Cells and Their Role in Regeneration
In case the blueprint is given in the ECM, the stem cells are the contractors that actualize it. The mesenchymal stem cells (MSCs) are the most versatile. Depending on the signals that they get out of the ECM, they can become cartilage, bone, or even connective tissue.
MSCs respond to the mechanical and biochemical cues of an ECM scaffold when grown on it. Their differentiation depends on the stiffness, texture, and composition of the growth factor of the scaffold. As an example, a more compact ECM stimulates osteogenesis (bone formation), whereas a less stiff matrix stimulates chondrogenesis (cartilage formation). However, these stem cells do not operate on their own. They are most active when there is PRP, a biological catalyst that makes them active.
According to studies published in Nature Scientific Reports (2025) and PubMed (2023), the combination of PRP and stem cells on ECM scaffolds enhances the survival of cells, the formation of the matrix faster, and of better quality in general.
It is due to this synergy that the modern regenerative therapies are so effective. The ECM provides guidance, the stem cells do rebuilding work, and PRP provides the fuel.
What PRP Really Does?
Platelet-Rich Plasma (PRP) might seem like a simple golden-yellow liquid that is withdrawn using a blood sample of a patient, but it has a powerhouse of regenerative capabilities. It is full of growth factors, including:
PDGF (Platelet-Derived Growth Factor): stimulates cell growth and tissue repair
TGF-β (Transforming Growth Factor Beta): regulates inflammation and promotes ECM synthesis
VEGF (Vascular Endothelial Growth Factor): triggers blood vessel formation
The addition of PRP on a stem-cell-loaded ECM scaffold converts the area into an active healing site. Growth factors, which enter the ECM, cause the attraction of the stem cells, increase their adhesion, and stimulate the synthesis of new collagen and elastin.
The increasing application of PRP in orthopedics, dermatology, and reconstructive medicine is supported by research provided by the Cleveland Clinic (2025) and JAMA (2022), which shows significant improvements in the time of healing, the quality of tissues, and patient outcomes. Precisely, PRP is the spark plug of the regeneration process, transforming an inactive scaffold into a living, biologically active system.
The Triad in Action: ECM + PRP + Stem Cells
The combination of ECM, PRP, and stem cells brings the phenomenon known to scientists as biological synergy. Each of these factors exaggerates the other:
- ECM acts as the scaffold, providing structure and signaling pathways.
- Stem Cells are the functional agents that read and respond to ECM cues.
- PRP delivers biochemical energy, activating growth and reducing inflammation.
Together, they establish a self-sustaining healing cycle, cells multiply, produce their own ECM, and eventually integrate into the body’s native tissue, completing the natural process of regeneration.
In a study published in Frontiers in Bioengineering and Biotechnology in 2025, the ECM + PRP + stem cell strategy was found to increase cartilage thickness by 40 percent and subchondral bone formation by mechanical stimulation compared to microfracture procedures.
The idea is more than mending, it is actual regeneration. This triad does not repair the damaged areas but creates tissue that is functionally and structurally the same as the original one.
Clinical Applications
Orthopedic Healing
PRP and stem cells embedded in ECM scaffolds are changing cartilage and ligament repair in orthopedics. The biologically active implants become stronger with time, which decreases inflammation and restores the natural movement of the joint.
According to the research findings presented in Frontiers in Materials (2022), ECM-stem cell-PRP complexes produce superior cartilage structure and morphology compared to traditional grafts.
Skin and Aesthetic Regeneration
In dermatology, ECM-based fillers enriched with PRP and autologous cells facilitate natural rejuvenation. They also cause lasting, biologically incorporated effects, unlike synthetic fillers, since they induce natural collagen production.
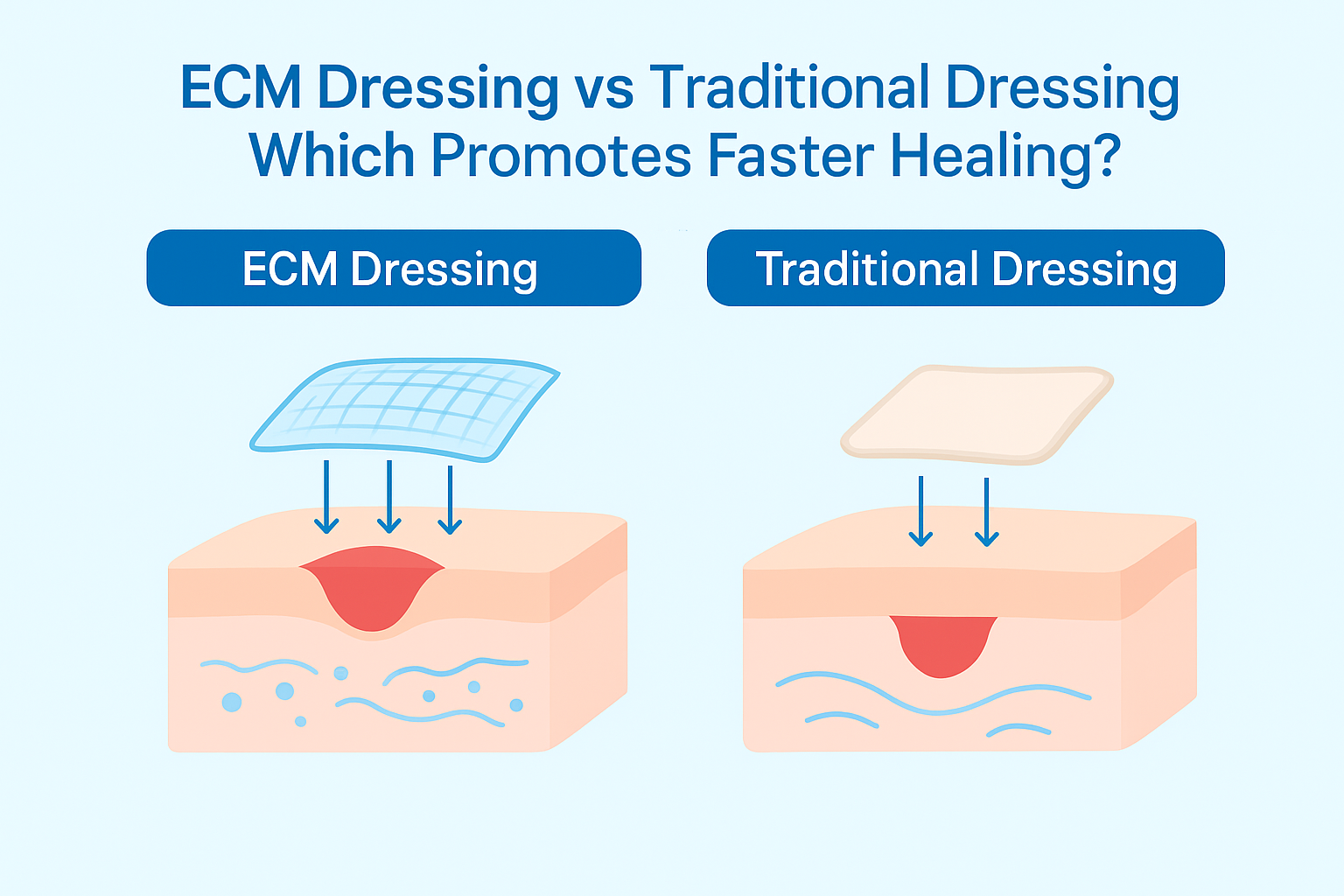
Chronic Wound Healing
ECM PRP-infused dressing is speeding up wound healing in diabetic and burn ulcers and decreases the risk of infection. In chronic care, the power of biologically informed scaffolds was demonstrated by a study conducted by a PMC (2020), where PRP-ECM dressings shortened the healing time by up to 40%.
Hardships and the Way Forward
The road to clinical perfection is yet to be built, even with the radical advances.
Technical Challenges:
ECM scaffolds printed or engineered using live stem cells need to be carefully controlled in regard to temperature, pressure, and oxygen. A single wrong factor can decrease cell viability. To eliminate the boundaries of nutrient diffusion, researchers are creating angiogenic bioinks and vascularized ECM models (MDPI Bioengineering, 2024).
Regulatory Barriers:
The FDA in the U.S. categorizes combined ECM-cell-PRP products as HCT/P combination devices, in which biologic and device approval are required (FDA.gov). Price, customizations, and ongoing experiments are the main challenges, but innovation is fast-growing.
According to the example set by Nature Biotechnology (2025), AI-controlled bioprinters are already automating the delivery of cells, and standardized ECM inks allow on-demand printing of objects at a hospital.
The Future
Imagine that you break your knee, but rather than getting an implant, which is made of metal, your doctor 3D prints a living graft using your own stem cells, PRP, and ECM proteins. The implant is not only perfectly shaped to your body, but also forms part of your body after weeks, leaving no residual or foreign substance.
This isn't far away. Stanford Medicine and the Mayo Clinic already test patient-specific ECM grafts in a very early phase of clinical trials. The future of PRP and stem cells is in personalization, where medicine does not fix what is broken; instead, it trains your body on how to fix it better.
Conclusion
Combining PRP and stem cells will unleash amazing healing possibilities, but it’s the ECM that makes this alliance intelligent. The ECM mediates the interaction between cellular behavior and tissue structure by playing the roles of scaffold and signal hub.
All three (ECM + PRP + stem cells) are a transition from artificial repair to collaborative regeneration: technology and biology as one.
The goal is no longer just to fix the body, but to help it relearn how to heal itself naturally.
Frequently Asked Questions (FAQ)
What is the outcome of PRP + Stem Cells?
PRP plus stem cells is a combination of powerful synergy. PRP does, on the other hand, provide the growth factors that stimulate your stem cells and in turn, your stem cells promote tissue recovery. Combined, these promote healing and enhance structural recovery.
What is the role of the ECM in regenerative medicine?
The ECM provides the essential biochemical cues and natural framework needed for proper stem cell differentiation. Without it, the healing process would become disorganized and incomplete, lacking the structure necessary for true regeneration.
Is PRP safe to be used together with stem cells and ECM scaffolds?
Yes. PRP is a self-derived product and therefore has few chances of rejection. It is commonly used together with stem cells and ECM-based implants in practice (Cleveland Clinic, 2025).
Are PRP and stem cells able to heal arthritis-damaged joints?
According to preliminary findings by the Frontiers in Bioengineering and Biotechnology (2025), ECM-controlled PRP-stem cell treatment has the potential to regenerate cartilage volume, as well as enhance joint performance.
When will personalized ECM-based grafts be available?
Some hospitals are already testing patient-implants of bioprinted cartilage, such as Mayo Clinic and Stanford Medicine. It will require 5-10 years to be used in the mainstream.
Is there any ethical issue with the use of stem cells?
In most cases, the material (in regenerative therapies) are adult cells whether from bone marrow or fat tissue and not embryonic sources." This method renders their application ethical and sustainable, aligning with modern medical and ethical standards.


.png)

.webp)


.webp)
.png)