How ECM Biomaterials Help Close the Gap in Diabetic Foot Ulcer Treatment
Learn how ECM biomaterials are treating Diabetic Foot Ulcers to promote growth, tissue regeneration and the rebuilding of healthy skin.
Diabetic foot ulcers (DFUs) are one of the most dreadful complications in diabetic patients, causing serious infections that lead to amputations and death if not treated. Although there has been noticeable progress in the field of wound healing and cutting-edge medicines, millions of patients worldwide are affected with diabetic wounds that refuse to heal by using conventional approaches such as gauze dressings, topical antibiotics, and negative pressure on the wounds.
This common problem has motivated researchers and practitioners to search for regenerative remedies that go beyond mere covering of the wound, that can actually restore, rebuild, or regenerate the tissue devastation. Among these innovations stands out the one of the most promising technologies that has come from this has been extracellular matrix (ECM) biomaterials, which have transformed chronic wound healing by enabling full-thickness ulcer closure for diabetic foot ulcers.
Understanding Diabetic Foot Ulcers
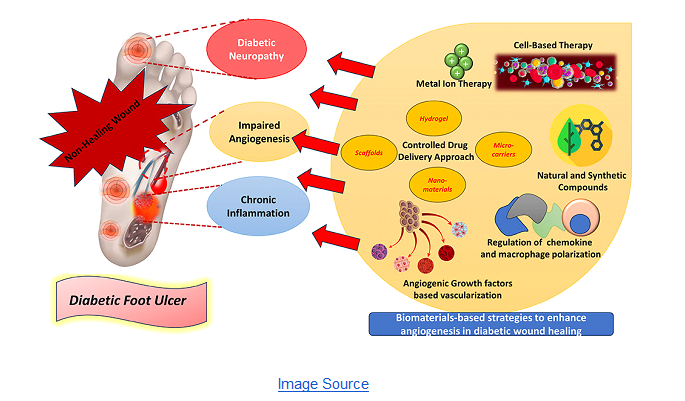
Diabetic Foot Ulcers and Open Wounds Diabetic foot ulcers are sores or wounds, usually located on the soles of the feet. They are mainly due to a combination of peripheral neuropathy (damage to the nerves in your feet), poor blood circulation, infection and pressure points resulting from deformities in the foot. Further studies show, “Diabetic foot ulcers (DFU) are a debilitating and life-threatening complication of Diabetes Mellitus. Ulceration develops from a combination of associated diabetic complications, including neuropathy, circulatory dysfunction, and repetitive trauma, and they affect approximately 19–34% of patients as a result.”
Healing is markedly impaired in diabetic patients. Elevated blood glucose levels result in impaired immune response, reduced collagen synthesis and diminished angiogenesis. These tend in combination to retard or prevent wound repair. Eventually, a little blister or cut could grow to become a chronic, non-healing ulcer.
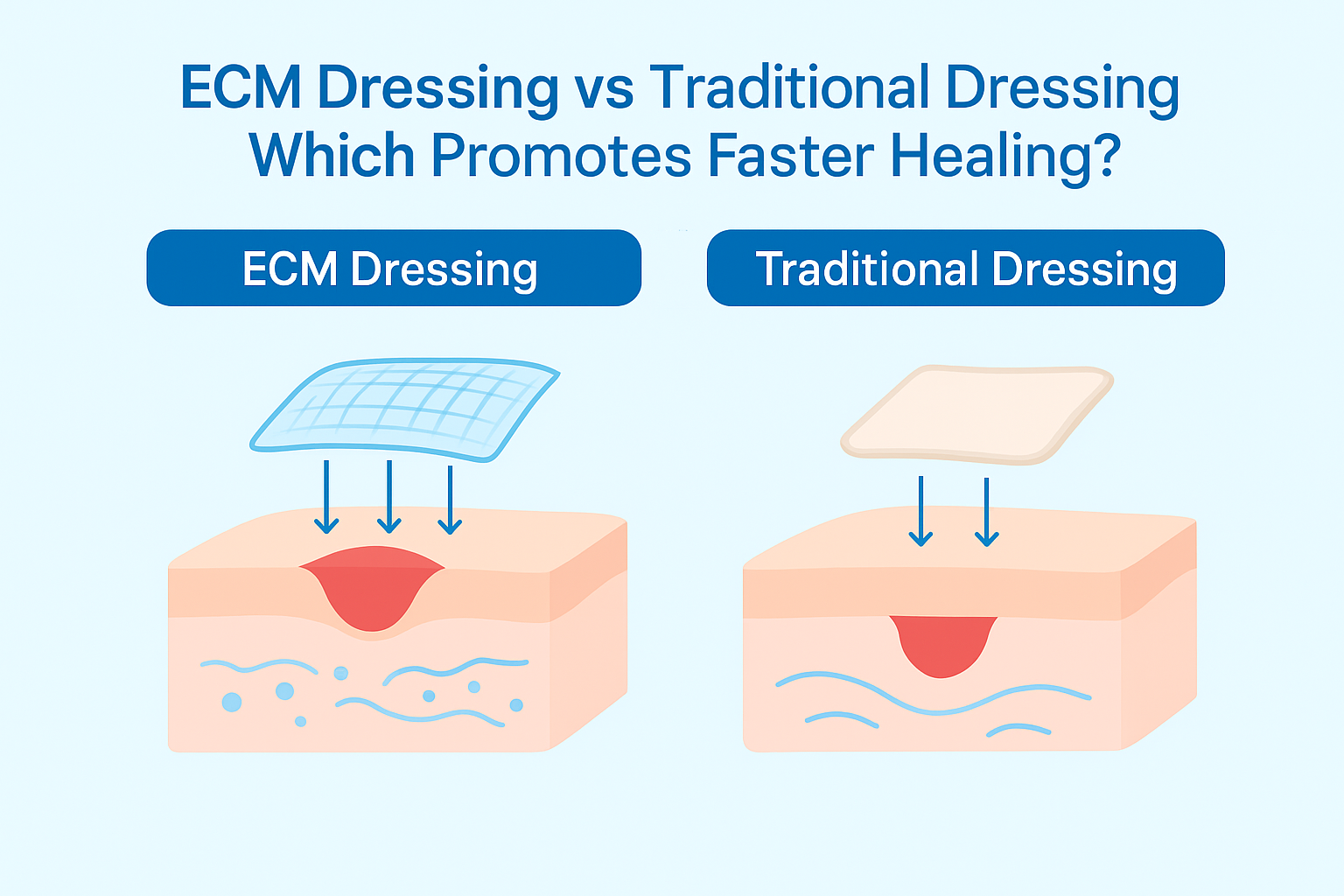
Conventional wound management focuses on cleansing, debridement, infection management, and the application of protective dressings. Nevertheless, these strategies do not restore the biological deficiencies that fail in healing in diabetic patients. This is where ECM biomaterials become involved to provide a regenerative strategy by targeting not only the entire surface but also the microenvironment of the wound.
What Are ECM Biomaterials?
The ECM is a tridimensional network of proteins, glycoproteins and polysaccharides that provides structural and biochemical support to the associated cells in virtually all organs. It’s the natural “scaffold” that cells use to attach, communicate, and regrow.
ECM biomaterials used in medical science for tissue engineering purposes (such as SIS, bovine dermis, or human placental tissue) are acellular/Sterile and are derived from natural tissues that have undergone decellularization, meaning the removal of cellular material to extract only the structural matrix. This matrix preserves bioactive molecules such as collagen, elastin, laminin, fibronectin and growth factors which guide cellular migration, proliferation, and differentiation at the wound site.
For a diabetic ulcer, ECM biomaterials serve as a biological scaffold that supports recolonization and remodeling of the patient’s own cells to restore the wound to healthy native tissue. In contrast with synthetic wound dressings, ECM products are biocompatible, biodegradable and bioactive - they don't just cover up the wound- they contribute to the healing site.
How ECM Biomaterials Work in Diabetic Foot Ulcers
The healing of chronic wounds such as DFUs consists of various stages including inflammation control, cell migration, tissue formation and remodeling. ECM bioactive materials enhance all of these stages by modulating the wound bed environment.
Restoring the Natural Healing Environment
Chronic wounds are commonly stuck in an extended state of inflammation with high levels of proteases and low oxygenation. ECM biomaterials are one of the tools we can use to help create a more normal environment. Matrix collagen and glycoproteins scavenge surplus proteases, diminish inflammation, and serve as a matrix where new tissue develops.
Encouraging Cell Migration and Angiogenesis
One of the biggest issues with diabetic ulcers is reduced angiogenesis, or the growth of new blood vessels. ECM scaffolds secrete biochemical signals that recruit fibroblasts, keratinocytes and endothelial cells to the wound. These cells are indispensable in the development of granulation tissue and neovascularization, during which oxygen and nutrients can be supplied to the site of injury.
Supporting Tissue Remodeling
With the advent of healing, ECM biomaterials still aid in remodeling by helping organize new collagen fibers and extracellular components in such a way that they approximate normal skin. This mechanism reduces scarring and enhances the mechanical strength of healing tissue.
Delivering Growth Factors Naturally
Unlike topically applied growth factor approaches, which readily degrade, ECM materials maintain endogenously bound growth factors such as VEGF, FGF and TGF-β that are released slowly as the material degrades. This sustained release contributes to a longer duration of healing and tissue integrity.
Advantages of ECM Biomaterials Over Traditional Dressings
Although typical dressings such as gauze, hydrocolloids and foams provide mechanical protection against infection and help to promote wound fluid homeostasis, they do not biologically interact with the Wound. However, advantages that make ECM biomaterials more suitable for chronic wounds like diabetic foot ulcers include:
- Regenerative Healing: ECM dressings help heal by regenerating tissues, not just forming a scar.
- Biocompatibility: They can blend well with host tissue without inducing immunological rejection responses.
- Immunomodulation: ECMs suppress inflammation and decrease chronic inflammation at the site of injury.
- Improved Cell Signaling: They talk to the patient’s underlying cells, telling them to heal.
- Rapid Healing and Fewer Complications: There is clinical evidence to suggest that ECM dressings result in accelerated healing rates with a lower rate of infection or amputation.
Clinical Evidence Supporting ECM Biomaterials in DFU Treatment
The efficacy of ECM-based biomaterials in curing DFUs has been verified by a number of studies and clinical trials.
A randomized controlled trial, for example, showed that diabetic patients treated with porcine small intestinal submucosa (SIS) derived ECM had statistically higher complete wound closure rates than those receiving standard dressings. An article published in 2 October 2025 shows that wound healing involves hemostasis, inflammation, proliferation, and remodeling, with cells releasing cytokines and growth factors. In diabetic wounds, impaired angiogenesis, prolonged inflammation, oxidative stress, and neuropathy disrupt ECM formation. During remodeling, type I collagen accounts for 80–90% of the new matrix. ECM biomaterials can restore the wound environment, support tissue formation, and accelerate closure.
Human tissue derived ECM devices including amnion or placental based products have also been investigated for their strong regenerative and antimicrobial effects. These products contain high amounts of hyaluronic acid and anti-inflammatory cytokines, so the cream is excellent for diabetic patients who have poor immune responses.
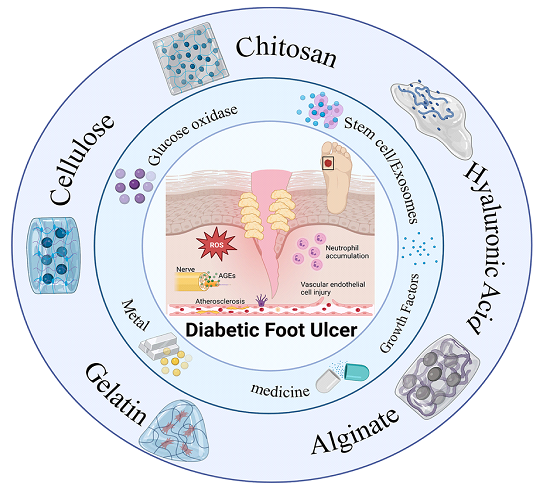
Different Types of ECM Biomaterials Used in DFU Care
- SIS (Porcine Small Intestinal Submucosa): One of the best-characterized and most widely used ECM scaffolds, that brings both structure and bioactivity.
- Bovine Collagen Dermal Matrix: Adds mechanical strength and support to larger wounds.
- Human Amniotic Membrane: Natural growth factors and anti-inflammatory proteins make this product ideal for fragile wounds.
- UBM (Urinary Bladder Matrix): Aids in revascularization and supports the return to a native skin matrix.
- Placental ECM Products: Demonstrates high biocompatibility and may be able to facilitate the healing of difficult ulcers.
All ECM types differ in physical and biological characteristics, enabling the clinician to select the type that matches size, depth of the wound, and patient status.
Growing Acceptance and Success in Clinical Practice
Use of ECM biomaterials in diabetic wound healing There has been an extraordinary increase in the use of ECM materials for the last decade. Today, even hospitals and specialized clinics around the world are integrating ECM-containing dressings in their treatment protocols. Their materials are tried, tested and proven to be one of the most reliable and scientifically supported solutions in regenerative wound care on the market.
Physicians have seen a reduction in healing time, complications and overall better patient satisfaction. And, with decreased rates of relapsed procedures and amputation there is long term health care savings to the system and better quality of life for the patient.
It is increasingly common for healthcare practitioners to perceive ECM biomaterials as more than simply advanced therapy, but rather a mainstream solution that connects historic wound care with today’s regenerative medicine. With increasing recognition, ECM-based products become the predominant treatment for DFUs in countries all over the world.
The Future of ECM-Based Diabetic Wound Care
The incorporation of ECM biomaterials in the management of DFU is undoubtedly a break through that shifts the focus from conventional wound care to regenerative medicine. In the future, ECM materials may be developed jointly with stem cells, exosomes, or bioengineered growth factors to expedite healing.
Furthermore, intelligent ECM dressings that can measure pH, temperature, or bacterial burden are currently under investigation. Such smart materials might give doctors instant feedback and adapt individual therapies for diabetics.
The hope is that ECM-based biomaterials can heal chronic wounds and contribute to eradicate those potentially life-threatening conditions by achieving complete skin linkage and vascular health.
Frequently Asked Questions:
⦁ What Is the Role of the ECM in Wound Healing?
The extracellular matrix (ECM) is a major player in wound healing as it creates a structural mesh, which allows the cells to attach and migrate while facilitating tissue regeneration. It normalizes the wound environment by providing critical biochemical signals to modulate fibroblasts, keratinocytes, and endothelial cells which are necessary for new tissue growth and angiogenesis.
⦁ How to Close a Diabetic Foot Ulcer?
Closing a diabetic foot ulcer requires proper wound care and diabetes management. Treatment includes cleaning and debriding the wound, maintaining moisture with ECM- or collagen-based dressings, and off-loading pressure using special footwear. In severe cases, skin substitutes, negative pressure therapy, or surgery may be needed, along with strict blood sugar control.
⦁ What Are Collagen-Based Biomaterials for Wound Healing?
Collagen-based biomaterials are advanced dressings made from natural collagen, a key protein of the extracellular matrix. They support new tissue growth, attract healing cells, and maintain a moist wound environment. Available as sheets, gels, or powders, they’re highly effective for chronic wounds like diabetic foot ulcers and burns.
⦁ What Are the Benefits of ECM-Based Wound Dressings?
ECM-based wound dressings help accelerate healing by restoring the natural environment needed for tissue repair. They reduce inflammation, promote new cell growth, and support blood vessel formation. These dressings are biocompatible, minimize scarring, and are especially useful for chronic or hard-to-heal wounds.
⦁ What Is the Gold Standard of Treatment for Diabetic Foot Ulcers
The gold standard for management of diabetic foot ulcers (DFUs) centers on a multidisciplinary approach to include pressure off-loading of the ulcer, appropriate wound care, infection control and glycemic regulation. More advanced treatments such as debridement, dressings (including ECM-based) and occasionally skin substitutes or negative pressure wound therapy are utilized to encourage healing. Surveillance and patient education is also important to prevent recurrence.
Conclusion
Diabetic foot ulcers (DFUs) continue to be one of the most devastating and costly complications of diabetes, afflicting millions of people globally. Traditional treatments tend to disappoint because they do not better the biological rhythms that promote recovery. ECM biomaterials overcome this deficiency by forming a regenerative environment to induce cell growth, angiogenesis, and tissue remodeling, the key components for full and forever wound closure.
Due to their composition and bioactivity, ECM dressings actually are more than the higher-level wound dressings: They participate in tissue repair. Continued research to develop and improve on their utilities will see ECM-based biomaterials revolutionize the treatment of diabetic foot ulcers, providing patients with a new lease of life and hope.


.png)


.webp)


.webp)
.png)